IDAHO FALLS, Idaho — Jenny Steinke, 36, died of poverty.
Her mother-in-law, Clella, said that’s the most apt cause of death. Steinke’s asthma was treatable, according to the doctor who tried to save her. Without affordable care, Steinke resorted to short-acting inhalers. Relief waned as she used more; she died in September 2015.
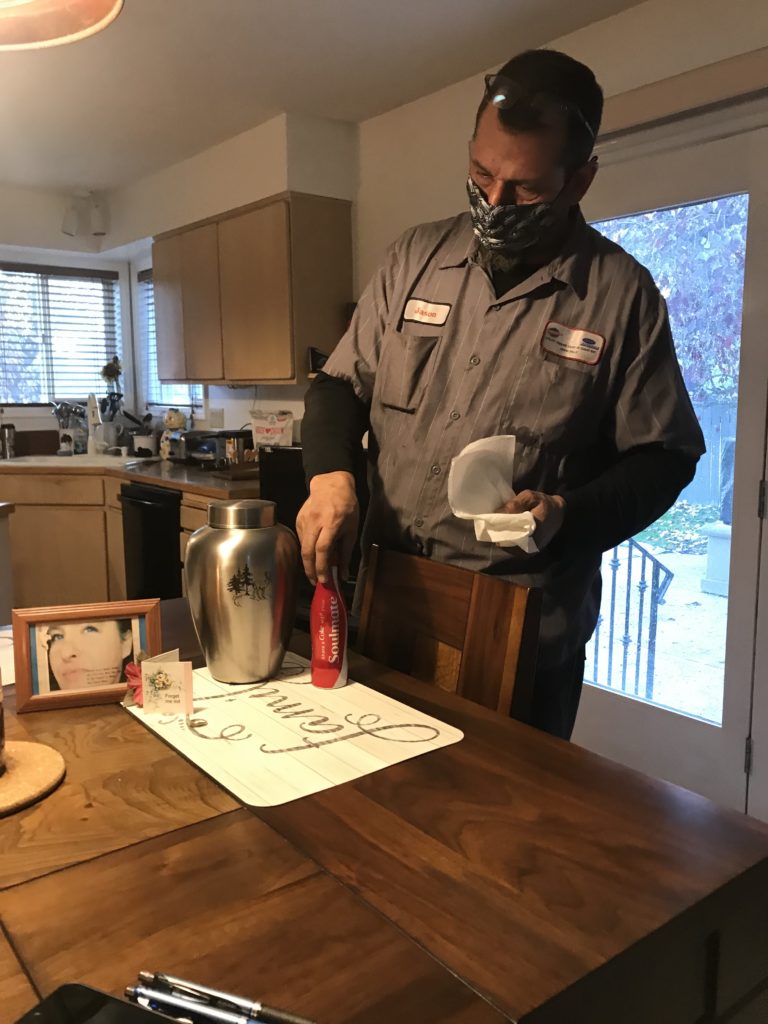
“It was preventable,” said Jason Steinke, his 6-foot-something frame slouched as he sat across the table from his wife’s brushed metal urn. He’d arranged Jenny next to a picture and metal Coke bottle inscribed “Soulmate.”
Jenny Steinke’s death became a rallying call for activists in the push to expand Medicaid in Idaho, where a Republican-majority Legislature refused expansion, in part, due to concerns that state taxpayers would be left to foot the bill if the federal government no longer wanted to pay for most of the policy. The lawmakers were also wary of policies that expand government.
Clella became an advocate. Newspapers covering expansion repeated her grim assessment of Steinke’s death — death by poverty. And Kenneth Krell, an Idaho Falls intensive care doctor who treated Steinke during her final days, pressed politicians along the way. Once, Krell even accused state lawmakers of killing 1,000 Idahoans by refusing to expand Medicaid.
Five years later, Krell is still in the public eye, nudging small-town public officials in reliably Red Idaho— last led by a Democratic governor in 1995 — toward scientifically-sound COVID-19 responses in a state where even rarely-enforced restrictions are a hard sell.
Related: ‘Enough with the masks!’: Behind Idaho’s struggle to contain the coronavirus surge
From the start of the pandemic, doctors across the state stepped in. They’ve become regulars at public meetings.
At first, eastern Idaho’s public health board was reluctant to issue mask mandates. A handful of doctors, including Krell, soon told the board that mandates were needed immediately.
“We don’t know how many cases we have,” Krell told the board in mid-July. “We don’t have time to wait. We simply don’t.” A spike was emerging then. Testing delays underrepresented its severity.
The next week, the health board issued the first county-level mandate. Over the coming months — as case counts grew, died down and grew again — it would issue, lift and re-issue mandates in all eight counties under its jurisdiction.
Half of Idahoans live in an area where masks are mandatory, according to the governor. But compliance with health guidelines isn’t as high as experts would like. The pandemic once seemed like a far-away issue for some remote communities in the largely rural state. Several times, vocal mask critics and virus skeptics in Idaho have made headlines for defying public health restrictions. A few instances have led to arrests.
Idaho’s governor, Brad Little, inched the state through his reopening plan this summer. He removed virtually all statewide restrictions, handing off most pandemic control to regional health officials.
Get the Latest Dispatches from across America
Sign up for our weekly On the Ground roundup
As hospitals across the state fill up lately, Little has restricted large gatherings and deployed the national guard to deal with hospital staff shortages. But he continues to refuse calls by health care leaders for a statewide mask mandate, saying that local responses are better.
Idaho is routinely listed in the “red zone” by the White House Coronavirus Task Force. Virtually every national coronavirus tracker says Idaho’s a hotspot. Hospitals from all corners of the state have had full ICUs last month. And Idaho, home to less than 2 million people, has had about as many COVID-19 deaths as Oregon, with over 4 million people.
Krell pleaded with Little in a letter he co-signed with 10 other Idaho hospital disaster planners in early November: “We strongly implore you, we beg you, to take the courageous step of immediately instituting a statewide, enforceable masking mandate,” they wrote.
In many ways, Krell’s demeanor today mimics the tone he struck while he pushed lawmakers to expand Medicaid.
Five months after Steinke died, Krell stood before a state Senate committee. He told Idaho lawmakers that, by refusing to expand Medicaid, they killed about 1,000 Idahoans over three years.
“Jenny’s case for me really crystalized what’s wrong here,” Krell said in February 2016. “And I kept asking myself, ‘How could this be? How could, in a state like Idaho where we care about each other, could I be seeing deaths and really damaging illness on a nearly daily basis?”

He rattled off possible reasons against Medicaid expansion — a state policy, which the Affordable Care Act encouraged by offering almost all the funding for, that raises the income cap for Medicaid eligibility from 100% of the federal poverty limit to 138% of the federal poverty limit. Krell said he could only come to one “inescapable” conclusion.
“That the Idaho Legislature is unfortunately responsible for those deaths,” he told lawmakers. “Our intransigence, in failing to pass Medicaid in for the last three years, has probably resulted in over a thousand deaths in this state.”
The committee chairman told Krell that if he or others lobbed accusations, they’d be gaveled down.
Krell’s remarks continued throughout the push to expand Medicaid. That fight culminated in November 2018, when 60.6% of Idaho voters approved expansion. It took effect this January.
Weeks later, Krell and other doctors were faced with a new health crisis: the coronavirus pandemic. Responding seemed politically vexing to some, but evidence kept emerging on the success of mask mandates.
Krell popped into eastern Idaho public health meetings many weeks, correcting common myths and providing updates on what he’s seeing in the region’s largest ICU.
“I don’t know how to keep my mouth shut,” he said in a recent interview.
Following that push to get Medicaid expansion on the ballot in 2018, the first policy passed directly by Idaho voters in over a decade, Krell seemed bittersweet in his celebration.
“It’s been three more years. That means another 1,000 Idahoans have died,” Krell said at a rally last February. “But we’re about to put an end to that.”
In the years since Jenny Steinke’s death helped fuel the fight, the Steinkes hadn’t seen their lives change as a result.
Insurance had always been out of grasp for the Steinkes. They didn’t make enough to qualify for tax credits on the state health insurance exchange, but they made too much to qualify for Medicaid. Activists have coined that “the gap,” and estimates say 59,000 Idahoans were in it.
“Medicaid expansion didn’t help Jason and me,” Clella said.
Just before Jenny died, Jason began a job with benefits. His insurance policy became effective Sept. 1, the day Jenny was rushed to the hospital.
“Six years ago, I needed ” Medicaid, Jason said.
Kyle Pfannenstiel covers rural healthcare in eastern Idaho for the Post Register. This dispatch is part of a series called “On the Ground” with Report for America, an initiative of The GroundTruth Project. Follow him on Twitter: @pfannyyy
 A version of this story appeared on USA TODAY on NOVEMBER 19, 2020
A version of this story appeared on USA TODAY on NOVEMBER 19, 2020

































